Skills
Data collection, data cleaning, descriptive data analysis, data visualization
Relevant Links
This project won the Ralph Kupka Prize 2024 for
outstanding and impactful Dutch research into bipolar disorder
Background and Overview
This write-up summarizes key findings from my published research in the Journal of the American Academy of Child & Adolescent Psychiatry. Please note that it is tailored for an industry audience, so certain details and nuances may be omitted. For a comprehensive understanding of the study, I encourage you to read the full paper, available here.
Reference: Helmink, F. G. L., Mesman, E., & Hillegers, M. H. J. (2024). Beyond the window of risk? The Dutch Bipolar Offspring Study: 22-year follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. doi:10.1016/j.jaac.2024.05.024
Understanding risk factors for severe mental health disorders is critical for early intervention and improved outcomes. For this study, we followed individuals at familial risk for bipolar disorder over a 22-year period — from adolescence into middle adulthood, tracking the progression of mood disorders and psychiatric symptoms. By analyzing long-term trends in mental health outcomes, we provide key insights into when individuals are most vulnerable and how risk evolves over time.
Data Structure Overview
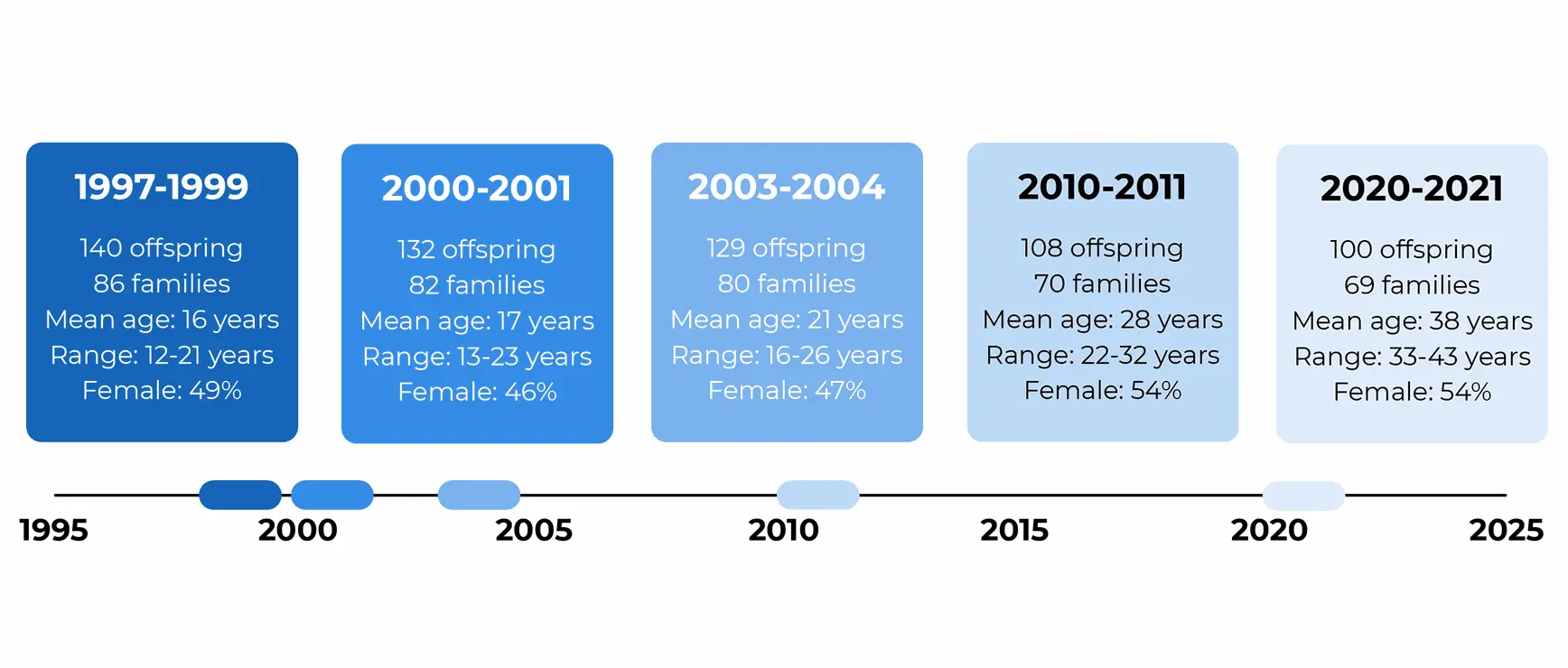
The data structure for this project is designed to support longitudinal analysis of offspring at risk for bipolar disorder, with five waves of assessment collected over 22 years. The key components of the data are as follows:
Cohort: The Dutch Bipolar Offspring Study
140 offspring of 86 parents with bipolar I (BD-I) or bipolar II (BD-II) disorder, ages 12-21 at baseline. A total of 100 offspring from 69 families still participated after 22 years (72% retention rate). At the 22-year follow-up, offspring had a mean age of 38 years (range 33-43 years) and 54% was female.
Mood Episodes
Collected data includes information on lifetime prevalence of psychiatric disorders, age of onset, number of episodes, and episode duration for mood disorders, with a focus on major depressive disorder and bipolar disorder.
These data allow us to examine lifetime and point prevalence, mood disorder trends across age, how one psychiatric episode can lead to another, and comorbidity.
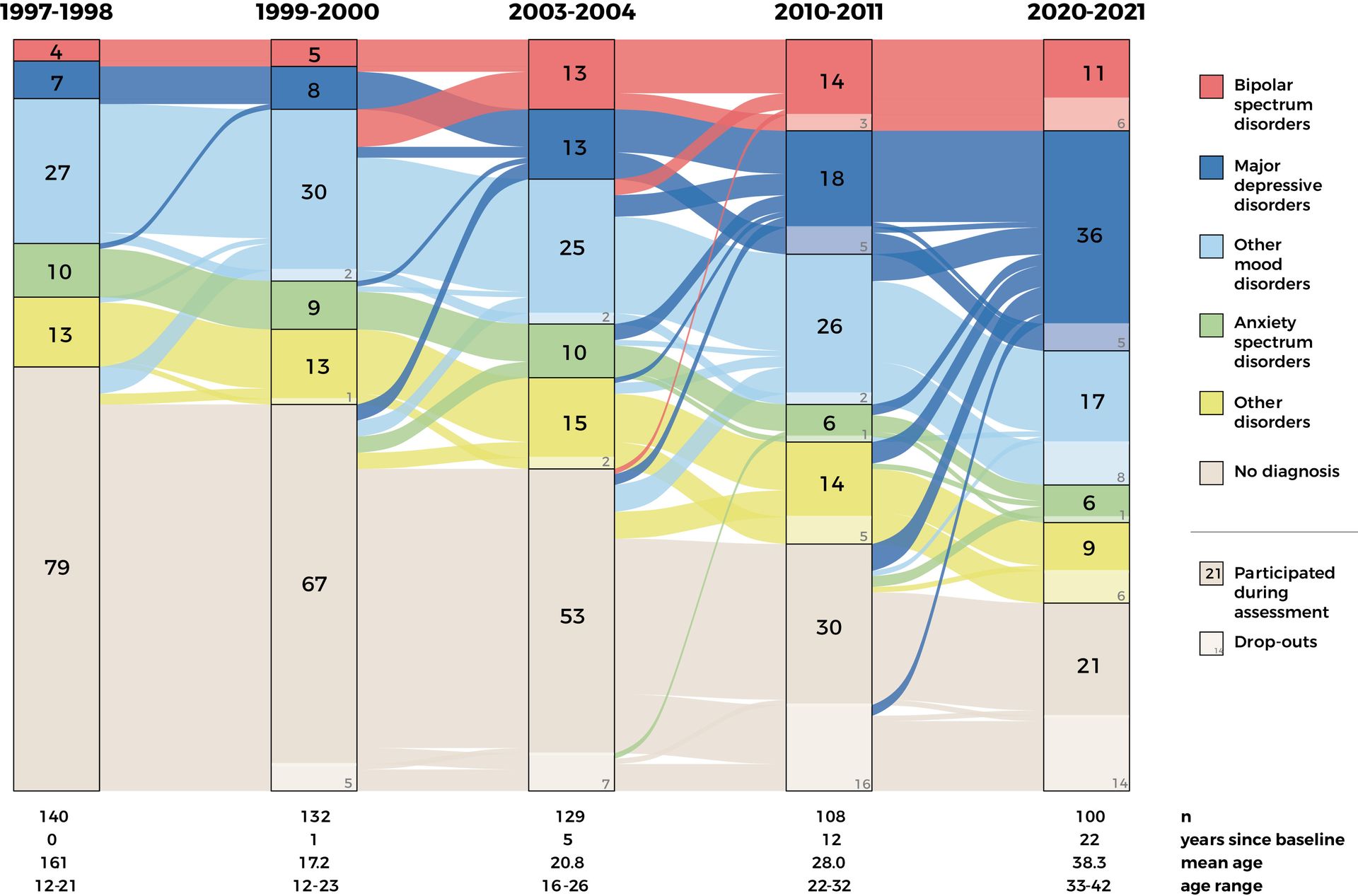
Longitudinal design of the Dutch Bipolar Offspring Study
Executive Summary
Individuals at familial risk of bipolar disorder are at significantly higher risk for psychiatric disorders, with 80% experiencing one in their lifetime, and 65% developing mood disorders—double the risk of the general population. The period between ages 20-25 shows the highest prevalence of psychiatric distress, highlighting a window of risk. This is strengthened by the lack of new bipolar disorder onsets after age 28. As mood disorders become more severe and recurrent with age, long-term support is needed to prevent further impairment.
Moreover, early screening remains important, particularly as 88% of those with bipolar disorder first experienced depression, with a diagnosis delay of 5.3 years.
Comorbidity is common, with 75% of those with mood disorders also having additional conditions such as anxiety (46%) or substance use (23%). To address this, integrated care models are essential, as they provide coordinated treatment for co-occurring disorders.
Policymakers should focus on early identification of at-risk individuals, age-specific interventions for young adults, and continuous mental health care throughout adulthood. These strategies aim to reduce the lifetime burden of psychiatric disorders and improve the well-being of individuals at familial risk of bipolar disorder.
Insights Deep Dive
#1 Prevalence of Lifetime Psychiatric Disorders
This study offers a rare, longitudinal glimpse into the mental health outcomes of individuals at high familial risk for bipolar disorder. By tracking participants from adolescence to middle adulthood, we uncover patterns that highlight both vulnerability and resilience. Below are the key insights and their broader implications:
1 | Prevalence of Lifetime Psychiatric Disorders
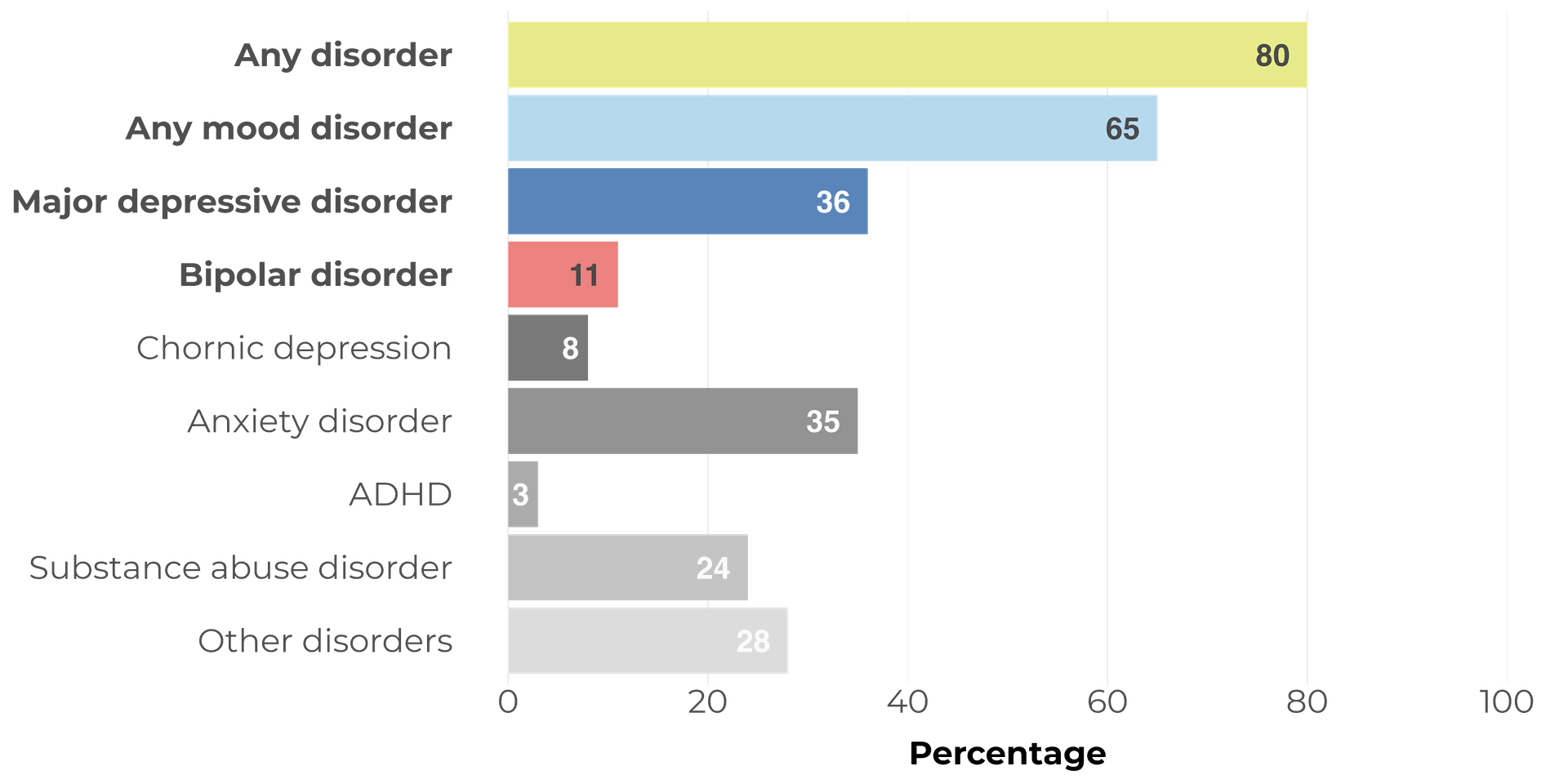
Looking at lifetime prevalence of psychiatric disorders in offspring of parents with bipolar disorder in middle adulthood (mean age 38 years) wil help us understand the lifetime risk that comes with intergenerational transmission.
- In total, 80% of the offspring developed any psychiatric disorder throughout their lives.
- The risk for any mood disorder was also high, with 65% having experienced at least one mood episode during their lives. This is at least 2 times the risk compared to the general Dutch population. [1]
- Over one third of offspring (36%) developed a major depressive disorder when reaching middle adulthood.
- Bipolar disorder was with its 11% prevalence not the most present in absolute terms, but the risk in the general population is 1-3%. This suggests that being at familial risk for bipolar disorder means the risk for developing bipolar disorder is three to ten times as high.
Prevalence of lifetime psychiatric disorders at mean age 38 years
Insights Deep Dive
#2 Increase Risk for Mood Disorders, But No New Bipolar Disorder Onsets
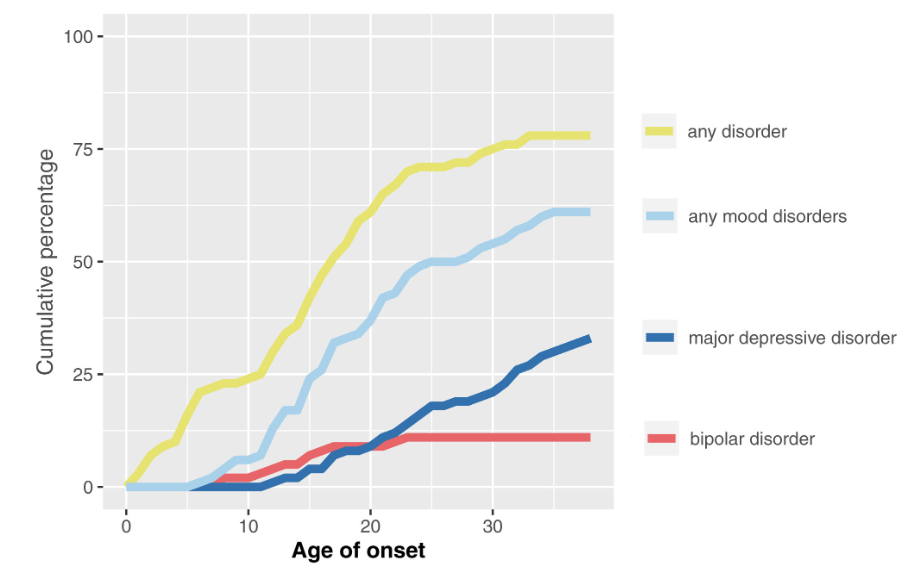
2 | Increased Risk for Mood Disorders, But No New Bipolar Disorder Onsets
- No new cases of bipolar disorder emerged after age 28, suggesting that bipolar disorder development largely stabilizes in early adulthood.
- Mood disorders became more prevalent over time, increasing from 54% to 65%, with major depressive disorder more than doubling (17% to 36%) since age 28, the time the fourth measurement took place.
- Adults who grew up with a parent with bipolar disorder face a heightened risk of mental health challenges, with new onset giving way to recurring and more severe episodes over time.
Cumulative rates of age of onset for psychiatric disorders
Insights Deep Dive
#3 The Young Adult Peak: A Critical Period for Intervention
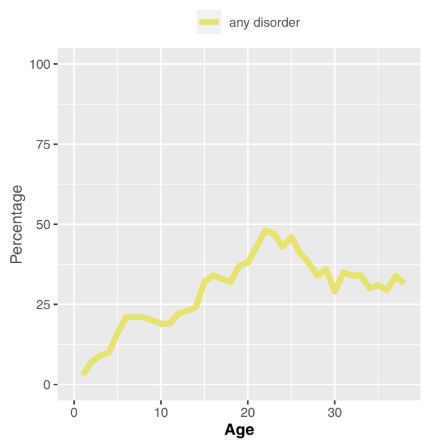
3 | The Young Adult Peak: A Critical Period for Intervention
Point prevalence shows the amount of individuals having a psychiatric disorder at any given point in time. In this case, at any given age.
- Point prevalence of any psychiatric disorder peaked between ages 20 and 25 (38%-46%) and remained substantial after age 30 (29%-35%).
- This supports that young adulthood is a particularly vulnerable period for psychiatric distress, even among individuals who do not go on to develop severe mental illnesses.
Age-specific prevalence of any present psychiatric disorder
Insights Deep Dive
#4 A Hierarchical Pathway: From Depression to Bipolar Disorder
4 | A Hierarchical Pathway: From Depression to Bipolar Disorder
- Among participants who developed bipolar disorder, 88% experienced a depressive episode first, with an average of 5.3 years between the first depressive episode and the onset of bipolar disorder symptoms.
- A total of 72% of those with major depressive disorder had prior psychiatric episodes, with one-third experiencing minor mood episodes before developing major depressive disorder.
Hierarchical Flow of Psychopathology From Baseline to 22-Year Follow-up
Note: Darker-colored blocks contain the total number for the respective psychopathology group. Lighter-colored blocks represent the number of dropouts that belonged to the respective psychopathology group at the respective assessment. Flow lines between the blocks indicate movement between psychopathology groups from time point T to time point T+1. The figure is a hierarchical reflection of psychopathology development, and participants belong to only one psychopathology group at one time point. In case of comorbidity, the highest in hierarchy was represented in this figure.
Insights Deep Dive
#5 High Comorbidity: The Challenge of Multiple Diagnoses
5 | High Comorbidity: The Challenge of Multiple Diagnoses
Comorbidity means having more than one illness or condition at the same time.
- Among those with any mood disorder, 75% had at least one comorbid condition, most commonly anxiety (46%) and substance use disorders (23%).
- This high comorbidity suggests that psychiatric disorders in offspring of parents with bipolar disorder rarely occur in isolation, making treatment more complex.
Recommendations
Early Screening
Early Screening
Early Identification of High-Risk Depressive Episodes
- Since 88% of individuals who developed bipolar disorder first experienced depression, clinicians should closely monitor depressive episodes in individuals at familial risk for signs of bipolar conversion.
- Screening for subtle bipolar symptoms (e.g., subthreshold hypomanic episodes, mood instability) during early depressive episodes could enable timelier interventions.
Reduce Delays in Bipolar Diagnosis & Treatment
- With an average of 5.3 years between first depression and bipolar onset, this window presents a key opportunity for proactive monitoring and intervention.
- Instead of a wait-and-see approach, mood disorder specialists should implement structured follow-ups for individuals with early-onset depression, particularly those with a family history of bipolar disorder.
Recommendations
Long-Term Support
Long-Term Support
Strengthen Long-Term Support for Mood Disorders
- With mood disorders increasing significantly over time (from 54% to 65%) and major depressive disorder doubling, mental health interventions should emphasize long-term relapse prevention, coping strategies, and access to continuous care.
- This highlights the need for sustained psychological and psychiatric support rather than short-term interventions.
Recommendations
Age-Specific Screening and Care
Age-Specific Screening and Care
Refocus Screening and Prevention Efforts Beyond Bipolar Disorder
- Since no new bipolar disorder cases emerged after age 28, screening efforts should prioritize early adulthood as a critical window for identifying and managing new cases.
- After this period, mental health support should shift focus to preventing relapse and managing recurring episodes rather than detecting new bipolar onsets.
Develop Age-Specific Interventions
- Since different life stages come with unique stressors, mental health programs should be tailored to the needs of young adults (academic/career stress, identity formation) and those in their 30s (work-life balance, long-term stability).
- Digital mental health tools, flexible therapy options, and peer-led programs could be effective ways to reach young adults.
Recommendations
Integrated Care
Integrated Care
Adopt Integrated Treatment Approaches
- Since 75% of individuals with mood disorders also have at least one additional diagnosis, treatment should move beyond single-disorder models toward integrated care that addresses multiple conditions simultaneously.
- Collaborative care models—where psychiatrists, psychologists, and addiction specialists work together—can provide more effective, coordinated treatment.
Expand Access to Dual-Focused Therapies
- Many existing treatment programs focus on either mood disorders, anxiety, or substance use, rather than addressing them together.
- Expanding access to evidence-based therapies like Cognitive Behavior Therapy for anxiety-mood comorbidity and integrated substance use treatment could lead to better outcomes and lower relapse rates.